MEET JASMINE: She was recently diagnosed with stage II (T2N1) HR+/HER2- eBC
Find out why KISQALI is right for her

Jasmine is a 54-year-old dentist and a beloved wife, daughter, sister, and friend. In her free time, she enjoys visiting local food and music fairs.
- During a routine exam, her gynecologist discovered a lump in her left breast and ordered a mammogram
- A biopsy revealed her diagnosis of HR+/HER2- eBC
- After surgery and radiation, she is now in remission
Discover more: download Jasmine's patient profile.
Jasmine's clinical evaluation
Age | 54 |
Menopausal status | Postmenopausal |
Clinical features |
|
Hormone receptor assay status | ER+/PR+/HER2- |
Gene expression profile assay results | 21 (Oncotype DX) |
ECOG PS | 0 |
Prior therapy | Lumpectomy; adjuvant radiation |
Current therapy | Hormone therapy |
DIAGNOSIS: Stage II (T2N1) HR+/HER2- eBC
Estimated risk of recurrence for patients with stage II HR+/HER2- eBC:
3-year risk of recurrence is based on iDFS outcomes among patients with HR+/HER2- eBC who received ET in select CDK4/6 inhibitor clinical trials. Data are from control arms only; no comparisons should be made between results from CDK4/6 inhibitor arms.1,2
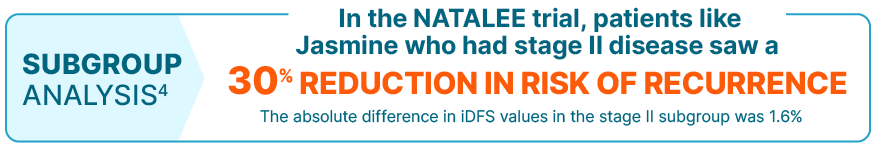
KISQALI consistently reduced the risk of recurrence in the broadest range of patients with stage II/III HR+/HER2- eBC
The iDFS benefit seen in the stage II subgroup was consistent with the overall population
Results from the subgroup analysis included no prespecified statistical procedure controlling for type 1 error.
iDFS was defined as the time from randomization to the date of the first event of local invasive breast cancer recurrence, regional invasive recurrence, distant recurrence, contralateral invasive breast cancer, second primary non-breast invasive cancer (excluding basal and squamous cell carcinomas of the skin), or death (any cause).3
NATALEE was a randomized, multicenter, open-label, phase III study of KISQALI + letrozole or anastrozole (n=2549) vs letrozole or anastrozole (n=2552) for the adjuvant treatment of men and women with stage II/III HR+/HER2- eBC. At a median follow-up of 33.3 months, with 509 iDFS (primary end point) events in the study (226 [8.9%] in the KISQALI arm and 283 [11.1%] in the NSAI-alone arm), iDFS at the 3-year landmark was 90.7% for KISQALI + NSAI vs 87.6% for NSAI alone (absolute difference 3.1%); there was a 25.1% relative reduction in the risk of an iDFS event; HR=0.749 (95% CI: 0.628-0.892). At a median follow-up of 38.6 months, iDFS for the prespecified stage II subgroup at the 3-year landmark was 94.2% for KISQALI + NSAI vs 92.6% for NSAI alone; HR=0.700 (95% CI: 0.496-0.986). Prespecified subgroups included anatomic stage (stage II: HR=0.700 [95% CI: 0.496-0.986]; stage III: HR=0.755 [95% CI: 0.616-0.926]), nodal status (N0: HR=0.723 [95% CI: 0.412-1.268]; N1, N2, N3: HR=0.759 [95% CI: 0.631-0.912]), menopausal status (premenopausal/men: HR=0.688 [95% CI: 0.519-0.913]; postmenopausal: HR=0.806 [95% CI: 0.645-1.007]), age (<45 years: HR=0.652 [95% CI: 0.443-0.959]; 45 to 54 years: HR=0.799 [95% CI: 0.578-1.104]; 55 to 64 years: HR=0.871 [95% CI: 0.636-1.193]; ≥65 years: HR=0.662 [95% CI: 0.444-0.986]), and histological grade at time of surgery (grade 1: HR=0.708 [95% CI: 0.303-1.657]; grade 2: HR=0.696 [95% CI: 0.548-0.885]; grade 3: HR=0.890 [95% CI: 0.658-1.204]). Grade 1 subgroup did not include patients with T2N0 disease. Results from the subgroup analysis included no prespecified statistical procedure controlling for type 1 error.3-6
KISQALI + AI consistently improved iDFS across subgroups, regardless of stage, nodal or menopausal status, age, or grade
KISQALI may be right for a variety of patients with stage II/III HR+/HER2- eBC.
KISQALI—approved for patients like Jasmine who have stage II N1 HR+/HER2- eBC with low genomic risk
See which patient types could benefit from KISQALI.
Patients with stage IIA, T2N0 HR+/HER2- eBC must meet the following criteria to be eligible for treatment with KISQALI: grade 3, or grade 2 with Ki-67 ≥20% or high genomic risk.6